Better for doctors.
Better for patients.
Increase patient engagement and utilization while minimizing disruption to prescriber workflow with myPrescryptive.

Capture and retain patients
Create a better and more effective prescription experience, right from the moment you welcome patients through your digital front door.
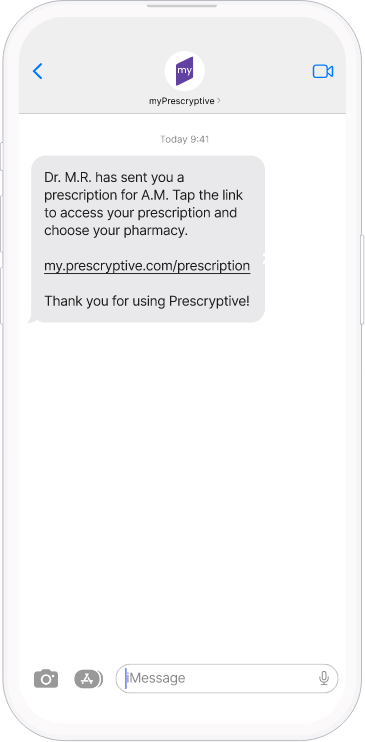
- Prescriptions are delivered right to the patient’s phone
- Make prescriptions actionable and build sustainable trust with patients through transparency and control
Increase adherence up to 11%
The costs of nonadherence and readmission are high, and not just for your patients.
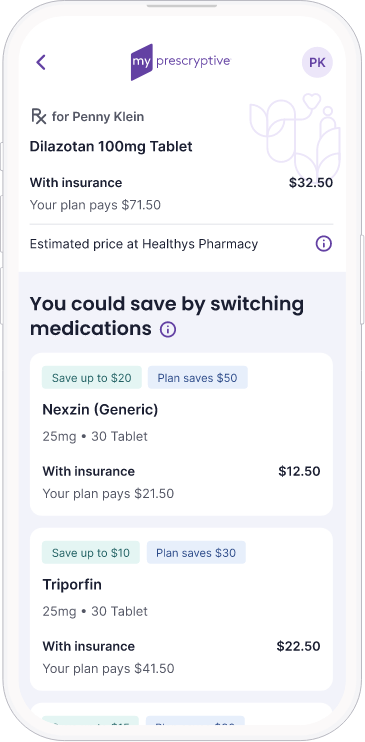
- Intelligent alerts help patients find better-priced alternatives and save money, helping to increase adherence
- Drive patients to the in-house pharmacy via shopping features and favorites
Empowered patients are healthier patients
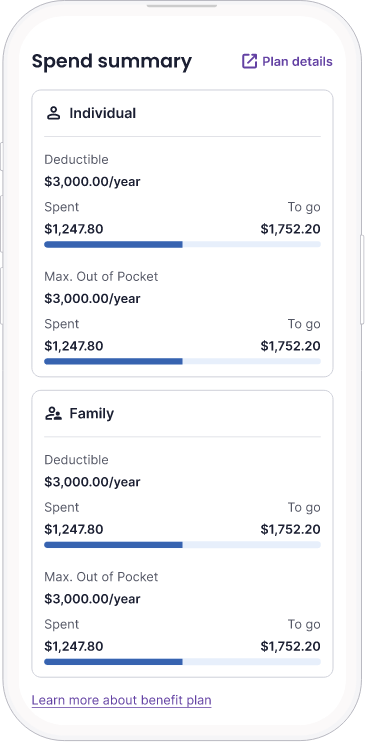
Our spend summary tool helps patients demystify their deductibles and take control of their spending.
- Transparency helps patients make informed decisions about how to pay for their medications
- Digital information helps connect patients to help drive up adherence, improve outcomes, and eventually lower the cost of care
Increase patient engagement
Better communication, more trusted information, and a sense of control over the prescription process helps build a deeper connection between your health system and its patients.
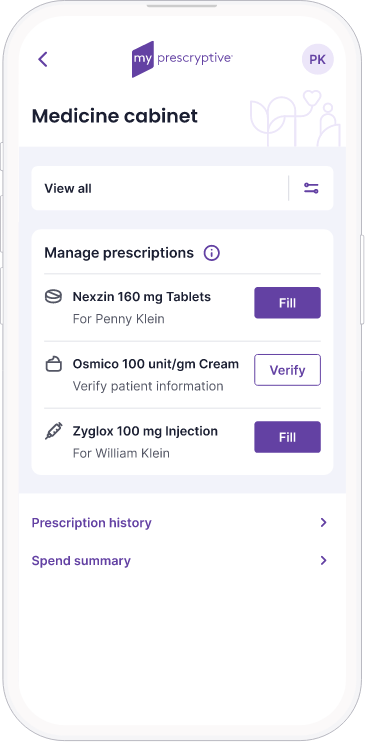
- Our digital medicine cabinet makes prescription management easy for individuals and families
- Every prescription is an opportunity to pull patients through a digital front door and increase patient engagement and retention
15%
bump in patient health record activations
11%
increase in patient engagement
60%
of first fills are abandoned for various reasons, including cost (IQVIA)
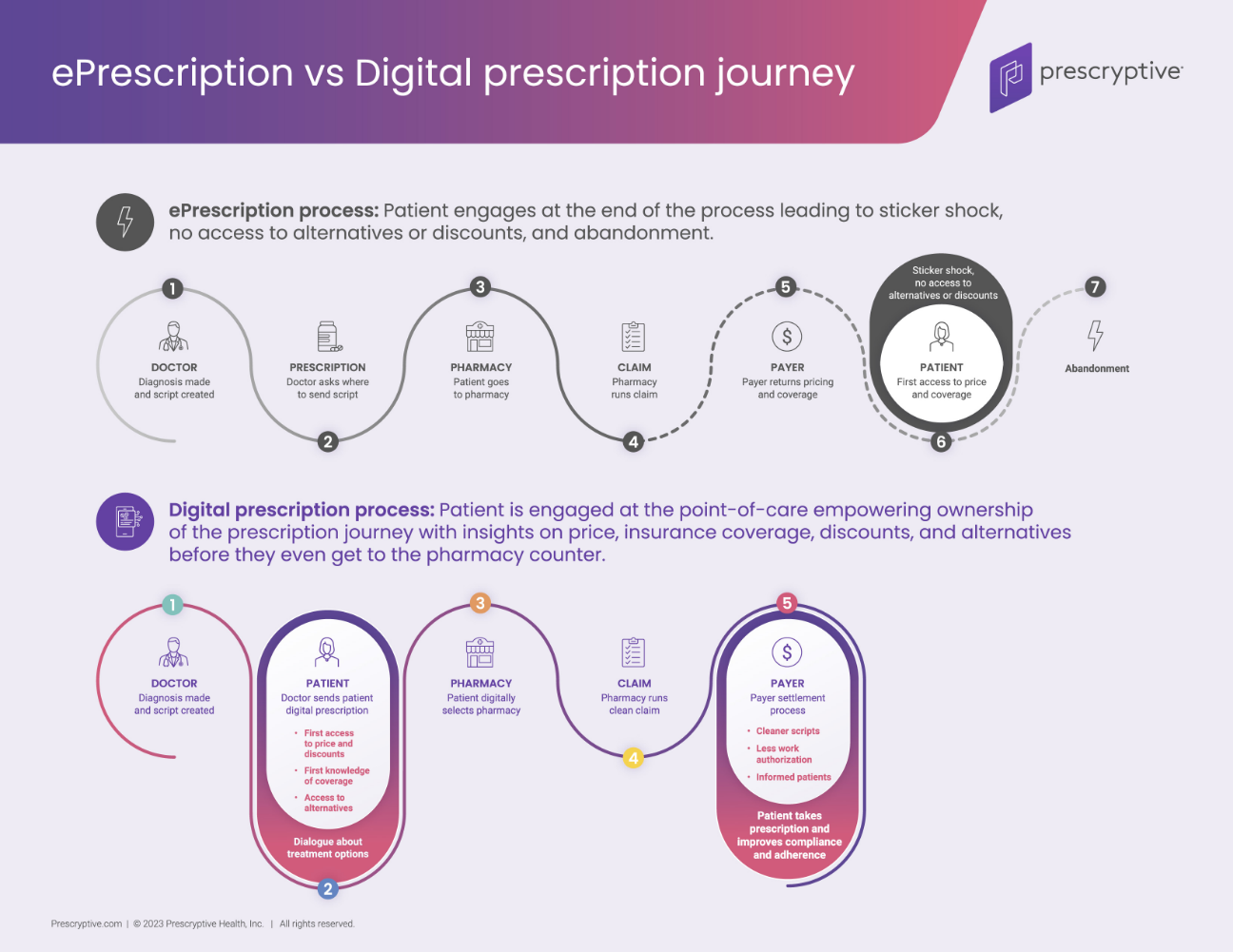
Our patented digital prescription technology creates new opportunities through:
- Removing the middlemen to change pharmacy economics
- Up to 250 hours saved per prescriber per year
- Using technology to empower and restore trust with patients

myPrescryptive + EHR
Capture and retain more patients, provide meaningful engagement opportunities, and support your digital strategy.
News & Insights
What is a digital prescription?
The days of paper prescriptions — when a patient got a piece of paper to carry from the…
Prescryptive named a Top 25 Healthcare Software Company by Healthcare Technology Report
The Healthcare Technology Report has named Prescryptive Health in the Top 25 Healthcare Software Companies of 2024. According…
2024 Health IT Predictions for Patients
Chris Blackley, CEO at Prescryptive Health, shares his insights for the year ahead: “Patients are demanding information and…
3 Ways Prescription Tech Will Impact Healthcare Organizations’ Bottom Lines in 2024
In 2024, health systems have an opportunity to improve patient experiences through prescription technology. Prescryptive’s SVP of Provider…
Connect with us
Want to bring transparency to your prescription process? Get in touch to see how.